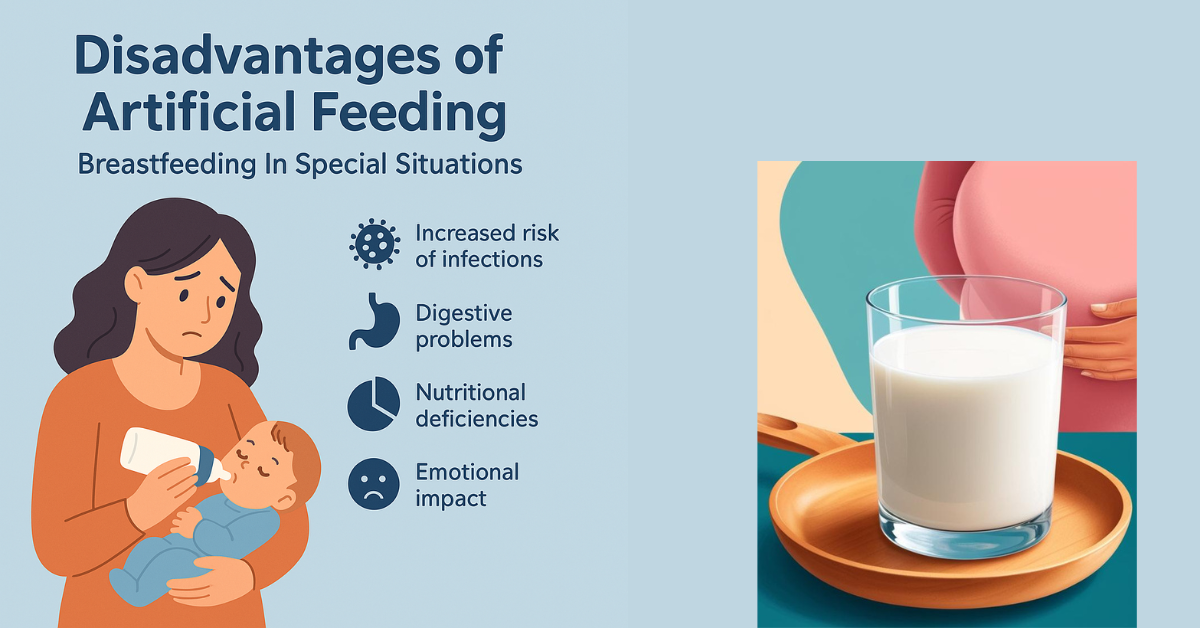
Disadvantages of Artificial Feeding Breastfeeding In Special Situations is a fundamental aspect of infant nutrition, providing numerous health benefits for both the mother and the child.
However, various challenges can arise during the breastfeeding journey, particularly for mothers of twins or infants with cleft lip or palate. Understanding these issues, including the disadvantages of artificial feeding, and implementing effective solutions is vital for promoting successful breastfeeding practices.
Disadvantages of Artificial Feeding Breastfeeding In Special Situations
Contamination Risks
One of the primary concerns with artificial feeding is the risk of contamination. Bottles and nipples that are not properly cleaned and sterilized can harbor bacteria, leading to gastrointestinal infections and other health issues for the infant. Unlike breast milk, which contains antibodies that help protect against infections, formula lacks these immune-boosting properties.
Nutritional Deficiencies
Artificially fed infants are more prone to nutritional deficiencies. For instance, animal milk does not provide the necessary living white blood cells and antibodies that breast milk contains. This can make formula-fed infants more susceptible to infections, diarrhea, and respiratory issues. Additionally, the iron present in animal milk is less bioavailable than that in human milk, potentially leading to anemia in formula-fed infants.
Cost Implications
The financial burden of artificial feeding can be significant for families. High costs associated with formula, bottles, and necessary supplies can lead some families to dilute formula to save money, which can compromise the nutritional intake of the infant.
Digestive Challenges
Artificial feeds can present challenges for an infant’s developing digestive system. For example, animal milk contains higher levels of saturated fatty acids and lacks essential fatty acids. Moreover, the high casein content can be difficult for an infant’s immature kidneys to excrete, leading to digestive distress.
Increased Risk of Infection
Supplementing breastfeeding with artificial feeding before six months can heighten the risk of infections and related complications. This underscores the importance of exclusive breastfeeding during the first six months of life, as recommended by health authorities.
Solutions for Ensuring Adequate Breast Milk
- Reassurance and Support: Healthcare providers should reassure mothers that they typically produce sufficient milk for their infants. Comfort during breastfeeding, including finding a relaxing position, can help stimulate milk production.
- Frequent Feeding: Encourage mothers to breastfeed frequently, both day and night. Increased sucking by the infant signals the mother’s body to produce more milk.
- Proper Latching Techniques: Educating mothers on correct breastfeeding positions and latching techniques can prevent pain and enhance milk extraction, promoting a successful breastfeeding experience.
Special Situations in Breastfeeding
Feeding Twins
Breastfeeding twins can be challenging but is entirely feasible. Most mothers have enough milk to nourish both babies, but they may need additional support.
- Feeding Strategies: Mothers can choose to breastfeed one twin at a time or simultaneously, depending on their comfort and the babies’ needs.
- Increased Support: Healthcare providers should reassure mothers about their milk supply and encourage them to nurse more frequently. This helps to establish and maintain an adequate milk supply.
Feeding Low Birth Weight Babies
Low birth weight babies may have difficulty sucking effectively, necessitating alternative feeding methods.
- Expressed Breast Milk (EBM): If the infant cannot suck, mothers should express milk several times a day and feed it using a cup or spoon.
- Skin-to-Skin Contact: Encouraging skin-to-skin contact (kangaroo care) can help stimulate the baby’s feeding instincts and improve overall health.
Feeding a Child with Cleft Lip or Palate
Breastfeeding infants with cleft lip or palate presents unique challenges. These conditions can make it difficult for the baby to create a proper seal for breastfeeding.
- Positioning: Holding the baby in a more upright position can help facilitate feeding.
- Specialized Feeding Tools: Some babies may benefit from using specialized bottles or teats designed for infants with cleft conditions.
- Expressed Milk: For infants who struggle to latch, feeding expressed breast milk through a cup or syringe can ensure they receive essential nutrients.
Breastfeeding a Sick Child
Breastfeeding should continue even if the child is ill, as breast milk is the most easily digestible food for an ill infant.
- Frequent Feeding: Encourage mothers to offer the breast more frequently, even if the baby appears to be sucking less vigorously.
- Comfort and Hydration: Breastfeeding provides not just nutrition but also comfort, which is especially important when a child is unwell.
Working Mothers and Breastfeeding
Returning to work can present significant challenges for breastfeeding mothers. Many mothers express concern about their ability to continue breastfeeding after returning to work.
- Breastfeeding During Work Hours: Whenever possible, mothers should consider bringing their infants to work or arranging for someone to bring the baby for feedings.
- Expressing Milk: Educate mothers on how to express breast milk effectively, so they can leave EBM for caregivers to feed the baby in their absence.
- Creating a Supportive Environment: Advocate for workplace policies that support breastfeeding, such as designated breastfeeding areas and flexible break times for nursing mothers.
Conclusion
Breastfeeding provides numerous benefits for both infants and mothers, yet various challenges can arise during this critical time. Understanding the disadvantages of artificial feeding and recognizing the specific needs of twins, low birth weight babies, and infants with cleft lip or palate are crucial for effective breastfeeding support.
Healthcare providers play a pivotal role in addressing these challenges by offering education, reassurance, and practical solutions. By fostering an environment that encourages breastfeeding and addressing concerns, we can significantly improve the health and well-being of mothers and infants alike.
Disadvantages of Artificial Feeding Breastfeeding In Special Situations
Disadvantages of Artificial Feeding Breastfeeding In Special Situations
Disadvantages of Artificial Feeding Breastfeeding In Special Situations
Read More:
https://nurseseducator.com/dialectic-teaching-with-team-based-learning/
https://nurseseducator.com/high-fidelity-simulation-use-in-nursing-education/
First NCLEX Exam Center In Pakistan From Lahore (Mall of Lahore) to the Global Nursing
Categories of Journals: W, X, Y and Z Category Journal In Nursing Education
AI in Healthcare Content Creation: A Double-Edged Sword and Scary
Social Links:
https://www.facebook.com/nurseseducator/
https://www.instagram.com/nurseseducator/