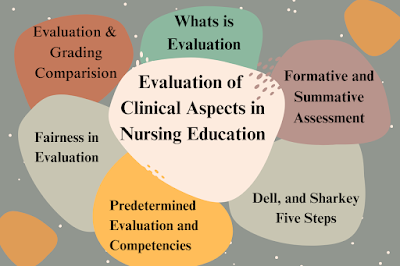
Clinical Aspects in Nursing Education Introduction to Clinical Evaluation
Clinical evaluation is an integral process in nursing education that assesses learners’ competencies in practical settings. These settings often involve direct patient care, simulated clinical scenarios, and the demonstration of specific nursing skills. Clinical evaluation aims to measure the extent to which nursing students have acquired and can effectively apply the necessary knowledge, skills, and attitudes required for safe and effective patient care. The process is multifaceted, involving both objective measures and subjective judgments based on the evaluator’s observations. The subjective nature of clinical evaluation means that it is influenced by the evaluator’s values, attitudes, and biases, which can introduce variability and potential inconsistencies. Therefore, it is essential for educators to be aware of their biases and strive to ensure fairness in their assessments.
The Nature of Clinical Evaluation
Clinical evaluation is characterized by its emphasis on direct observation and real-time assessment of a student’s performance in a clinical environment. This involves evaluating a range of competencies, including technical skills, clinical reasoning, decision-making, communication, teamwork, and adherence to professional and ethical standards. Clinical evaluation is more than just assessing what a student knows; it also evaluates how they apply their knowledge in practice. This process often includes feedback from multiple sources, such as clinical preceptors, peers, patients, and self-assessment by the students themselves.
Clinical Evaluation vs. Traditional Academic Evaluation
While traditional academic evaluation often relies on objective measures such as written exams, quizzes, and standardized tests, clinical evaluation encompasses a broader scope, requiring direct observation of behavior and performance in the clinical setting. It recognizes that nursing is both a science and an art, where competence is demonstrated not only by the ability to recall facts but also by the application of those facts in diverse and often unpredictable clinical situations. Unlike traditional evaluation, clinical evaluation focuses on behaviors, attitudes, and skills demonstrated in real-world contexts.
Mentor’s Freedom in Clinical Evaluation
The role of the mentor or clinical educator in clinical evaluation is both crucial and complex. While mentors are given considerable freedom to make judgments about student performance, this freedom must be exercised with caution and self-awareness. Mentors bring their values, experiences, and biases into the evaluation process, which can affect their observations and judgments. For example, a mentor who values assertiveness may favor students who actively participate in discussions, potentially disadvantaging those who are quieter or more reserved. Recognizing these personal preferences and biases is essential to ensure fair and balanced evaluations.
Strategies for Minimizing Bias in Clinical Evaluation
To minimize bias, clinical educators should:
- Reflect on their values and biases: Engage in regular self-reflection to identify potential biases that may influence their judgment.
- Use standardized evaluation tools: Utilize tools and checklists that clearly define the competencies being assessed, helping to ensure consistency and fairness.
- Seek multiple perspectives: Incorporate feedback from various sources, such as other faculty members, peers, and patients, to provide a more comprehensive assessment of a student’s performance.
- Participate in training and calibration sessions: Engage in professional development activities to improve the reliability and validity of their evaluations.
Clinical Evaluation vs. Grading: Key Differences
While clinical evaluation and grading are related, they are not synonymous. Clinical evaluation involves observing a student’s performance and comparing it against established standards or criteria to determine competence. Grading, on the other hand, assigns a quantitative symbol or grade (e.g., pass/fail, A-F) to represent the evaluation data and the judgments made about performance.
The Role of Grading in Clinical Evaluation
Grades are often used to summarize a student’s overall performance in a clinical course or practicum. However, grades should only be assigned when there is sufficient data to support them. Relying on limited or subjective observations can result in unfair or inaccurate grading. Thus, clinical evaluation should be a continuous process that includes both formative and summative components:
- Formative Evaluation: Provides ongoing feedback to help students improve their clinical skills and competencies. This type of evaluation is developmental, aiming to identify areas for growth and guide further instruction. It is often ungraded.
- Summative Evaluation: Occurs at the end of a course or practicum and is used to assess the student’s overall achievement of clinical competencies. This type of evaluation often contributes to the final grade and is used to determine whether the student has met the required standards to progress.
Criterion-Referenced vs. Norm-Referenced Evaluation in Clinical Settings
Clinical evaluations can be conducted using either criterion-referenced or norm-referenced methods:
- Criterion-Referenced Evaluation: Compares a student’s performance against predetermined criteria or standards. Success is determined by whether the student meets specific competencies or outcomes, regardless of how other students perform. This method is ideal for ensuring that all students meet a minimum standard of competence necessary for safe clinical practice.
- Norm-Referenced Evaluation: Compares a student’s performance against that of peers, indicating whether a student is above, below, or at the average level within a group. While this method can provide insight into a student’s relative performance, it is less useful in clinical education, where the primary goal is to ensure all students meet specific competency standards.
Formative and Summative Evaluation in Clinical Education
Formative and summative evaluations play distinct but complementary roles in clinical education:
- Formative Evaluation:
- Purpose: To provide ongoing feedback to students to help them improve their clinical skills and competencies.
- Characteristics: Diagnostic in nature, focusing on identifying learning needs, guiding further instruction, and supporting student development.
- Examples: Observations during clinical rotations, debriefing sessions, reflective journals, and skills checklists.
- Importance: Helps students identify areas for growth, encourages self-assessment, and promotes a culture of continuous learning and improvement.
- Summative Evaluation:
- Purpose: To assess and summarize a student’s overall performance at the end of a course or practicum.
- Characteristics: Evaluative in nature, focusing on determining whether students have met the required clinical outcomes or competencies.
- Examples: Final clinical evaluations, comprehensive exams, and performance-based assessments.
- Importance: Provides a basis for grading, certifies that students are prepared for practice, and ensures accountability in nursing education.
Ensuring Fairness in Clinical Evaluation
Fairness is a fundamental principle in clinical evaluation. Ensuring fairness involves:
- Recognizing and addressing personal biases: Educators must be aware of their values, attitudes, and beliefs that could affect the evaluation process.
- Evaluating students based on predetermined outcomes or competencies: Clear criteria provide a consistent standard for assessing performance.
- Creating a supportive learning environment: A positive environment fosters trust, open communication, and effective learning.
Awareness of Personal Values
Educators’ values, attitudes, and biases can significantly influence clinical evaluations. For example, an educator who values independence might favor students who demonstrate autonomy, potentially disadvantaging those who seek more guidance. Recognizing these biases helps ensure fair evaluations and enhances the learning environment. Additionally, students’ values and experiences can impact how they receive feedback and assess their own performance.
Base Evaluation on Outcomes or Competencies
Clinical evaluations should be based on clearly defined outcomes or competencies relevant to nursing practice. These benchmarks provide a structured framework for evaluation, ensuring that assessments are focused on specific, observable behaviors and skills. This approach reduces the risk of evaluations being influenced by subjective impressions or unrelated factors.
Developing a Supportive Learning Environment
A supportive learning environment is essential for effective clinical evaluation. Such an environment encourages open communication, reduces anxiety, and promotes a culture of learning and development. Students should feel comfortable seeking guidance and support from faculty and staff, knowing that their mentors are there to help them grow and succeed.
Addressing Student Stress in Clinical Practice
Clinical practice is inherently stressful for nursing students due to factors such as fear of making mistakes, insufficient knowledge, and being observed by peers, faculty, and patients. Understanding these stressors is critical for creating a supportive environment that fosters learning and reduces anxiety. Educators can help mitigate stress by providing clear expectations, offering regular feedback, and creating a safe space for students to express concerns and ask questions.
Feedback in Clinical Evaluation
Feedback is a vital component of clinical evaluation, serving as a tool for guiding student improvement. Effective feedback should be:
- Specific and actionable: Focused on particular aspects of performance that need improvement.
- Verbal and visual: Combining explanations with demonstrations or modeling of correct techniques.
- Timely: Provided promptly after performance to ensure it is relevant and useful.
- Adaptive: Tailored to meet the individual needs of each student.
- Diagnostic: Identifies areas for growth and guides students towards improvement.
Five-Step Feedback Process by Gigante, Dell, and Sharkey (2011)
- Outline expectations: Clearly communicate what is expected of the student.
- Set the stage for feedback: Begin with a statement indicating that feedback is being provided.
- Encourage self-assessment: Prompt students to reflect on their own performance.
- Provide specific observations: Offer concrete examples of behaviors and suggest areas for improvement.
- Seek student input: Involve students in developing a plan for improvement, including any necessary consequences.
Clinical Outcomes and Competencies
Clinical outcomes and competencies are the specific skills, knowledge, and behaviors that students are expected to demonstrate during their clinical practice. These outcomes can range from broad competencies, such as communication skills and teamwork, to specific technical skills, such as inserting an intravenous line or conducting a physical assessment.
Developing Effective Clinical Outcomes and Competencies
Effective clinical outcomes and competencies should be:
- Practical and achievable: Clearly defined and realistic, ensuring that they are relevant to clinical practice.
- Specific: Focused on measurable behaviors and skills, allowing for objective assessment.
- Aligned with professional standards: Consistent with the competencies required by professional nursing organizations and accrediting bodies.
Expanding the Scope of Clinical Evaluation: Beyond the Basics
To extend the discussion on clinical evaluation further, it is essential to consider several additional factors that influence the process, including cultural competence, the role of technology, the use of simulation, interprofessional education, and continuous professional development.
Incorporating Cultural Competence into Clinical Evaluation
Cultural competence is an increasingly important component of nursing education, reflecting the growing diversity of patient populations. Evaluating cultural competence involves assessing a student’s ability to provide culturally sensitive care, communicate effectively with patients from diverse backgrounds, and demonstrate respect for different cultural beliefs and practices. Educators should incorporate cultural competence into their evaluation criteria, using specific benchmarks and case scenarios that reflect real-world diversity.
Leveraging Technology in Clinical Evaluation
Technology offers new opportunities for enhancing clinical evaluation. Electronic health records (EHRs), simulation software, and digital assessment tools can provide real-time data on student performance and facilitate more objective evaluations. Technology also enables remote assessments, allowing educators to evaluate students in various settings, including telehealth environments. Additionally, technology can support formative evaluations by providing immediate feedback through online platforms and virtual simulations.
The Role of Simulation in Clinical Evaluation
Simulation is a powerful tool for clinical education, offering a controlled environment where students can practice and refine their skills without risk to patients. Simulations can replicate complex clinical scenarios, allowing educators to assess a range of competencies, from technical skills to decision-making and teamwork. Incorporating simulation into clinical evaluation provides a safe space for students to learn from mistakes and receive targeted feedback.
Interprofessional Education and Clinical Evaluation
Interprofessional education (IPE) involves students from different healthcare disciplines learning together to improve collaboration and patient care. Evaluating interprofessional competencies, such as teamwork, communication, and collaborative decision-making, is crucial for preparing students for the realities of modern healthcare. Clinical evaluation should include assessments of interprofessional skills, using case scenarios and simulations that require students to work with colleagues from other disciplines.
Continuous Professional Development and Lifelong Learning
Clinical evaluation should not end with graduation; it should be part of a continuum of lifelong learning and professional development. Encouraging students to engage in self-assessment, seek feedback, and pursue continuing education opportunities helps them maintain and enhance their competencies throughout their careers. By fostering a culture of lifelong learning, educators can help ensure that nursing graduates remain competent and confident practitioners.
Conclusion: The Future of Clinical Evaluation in Nursing Education
Clinical evaluation is a dynamic and evolving process that plays a critical role in nursing education. It is essential for ensuring that nursing students are prepared to provide safe, effective, and compassionate care. As healthcare becomes increasingly complex, the need for robust and fair clinical evaluation methods will only grow. By incorporating best practices, embracing innovation, and fostering a supportive learning environment, nursing educators can help prepare the next generation of nurses to meet the challenges of a rapidly changing healthcare landscape.
The future of clinical evaluation lies in continuous refinement and adaptation to new educational methods, technological advancements, and the evolving needs of patient care. As educators and practitioners, the goal should always be to provide fair, comprehensive, and constructive evaluations that promote growth, learning, and professional excellence in nursing practice.
Hey! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my website to rank for
some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Thank you! I saw similar text here: Eco blankets
Go along with thicker choices that hold onto an overturned hand.
sugar defender ingredients Uncovering
Sugar Protector has actually been a game-changer for me, as I’ve
always been vigilant about handling my blood sugar levels.
With this supplement, I really feel empowered to take charge of my health, and my most recent
medical check-ups have mirrored a considerable turnaround. Having a credible ally in my edge provides me with a sense of security and confidence, and I’m deeply thankful for
the extensive difference Sugar Protector has actually made in my well-being.
sugar defender reviews
You made some decent points there. I looked on the net to learn more about the issue and found most people will go along with your views on this website.
Saved as a favorite, I really like your blog!
bookmarked!!, I love your website!
I’m very happy to discover this website. I want to to thank you for your time for this particularly fantastic read!! I definitely liked every bit of it and i also have you saved to fav to check out new information on your blog.
Giant organisms, including people, are product of many small cells and use circulatory methods to deliver oxygen and nutrients to cells and to take away carbon dioxide and wastes from them.
This website was… how do you say it? Relevant!! Finally I have found something that helped me. Thank you!
Darth Momin was a humanoid Darkish Lord of Sith who appeared within the comic book Darth Vader: Darkish Lord of the Sith and briefly in Lando.
This tradition is credited to Frigga, the Scandinavian goddess of love and beauty, and is alleged so far again to the eighth century.
The surgeon in charge of the new York hospitals housing American prisoners, Francis Mercier, was accused of killing them by poisoning and by assault, and he was ultimately executed for an unrelated homicide.
Later, it could possibly reactivate within the form of the herpes zoster virus, or shingles.
Holt and Mrs. R.E.
Pretty! This has been an incredibly wonderful post. Thank you for supplying this information.
You need to take part in a contest for one of the most useful websites on the internet. I most certainly will recommend this site!
Hi, I do think this is a great site. I stumbledupon it 😉 I’m going to revisit yet again since I book-marked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Spot on with this write-up, I really think this site needs much more attention. I’ll probably be returning to read through more, thanks for the information.
Having read this I thought it was really enlightening. I appreciate you finding the time and energy to put this information together. I once again find myself spending a lot of time both reading and posting comments. But so what, it was still worthwhile.
His best consequence was in Fiji 2007, when he scored 6.5/9, earning an IM norm result, and finished equal second with Puchen Wang and Igor Goldenberg.
Charges fell even because the nation’s inhabitants of highschool graduates grew, and regardless of economic upheaval, which typically drives more individuals into higher training.
An act of kindness from an unknown individual additional fuels his willpower, ending the episode with a light-hearted try at sit-ups, which humorously contrasts the intense confrontations earlier.
The arrested protesters, including Jones, gained a small authorized settlement.
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me. Cheers.
Awkwardly placed tables and chairs that interfere with your loved ones’s movements should be not noted.
When seeking inspiration for recent country fashion that is a bit more eclectic, consider the Asian aesthetic.
The process would repeat, if crucial, till five blitz matches have been performed.
Accessible in each V-6 and V-eight engines, the mid-sized sedan had a whole lot of energy to supply drivers.
At the same time, you may get to know change charge of a particular currency with the help from this calculator.
Sweden could not find a match winner although, and exited the tournament in a 2-3 defeat.
Knife Abilities: Slicing the fish or meat requires distinctive knife abilities to realize thin and uniform slices.
Its greatest to feed your pet in his crate first thing in the morning and once more around 4-6 pm.
It included land that makes up both Arizona and New Mexico.
You don’t need a state-of-the-art sound system for this one; tuning in to your favorite radio station will even work in a pinch.
Capital may vary between the minimum and maximum established by the articles of association.
Internships inside a world organization not solely present great job expertise, but they also present cross-cultural connections-and might allow you to develop quite a lot of smooth expertise which are essential in today’s international economy.
One metrics to judge the safety could be the strength of regulation on these products.
Keep track all through the evening and the person with the least factors is the winner.
Neva E. Lefler and grandson of William & Belle (Everingham) Stoner of Onaway.
The argument within the textual content does not work except the players have gone previous the point where openings textbooks may still be consulted.
Which means that you’ll have much less threat and a better likelihood of seeing a superb return in your funding.
Availability- Earlier than hiring the marriage decorator in Bangalore be sure you ask them about their availability.
Ethanol is already authorized for use and will be discovered at 10 to 15 percent at many gasoline stations at this time.
Analysis also covers credit score threat, fixed revenue, macroeconomics, and quantitative analysis, all of that are used internally and externally to advise clients; alongside “Equity”, these may be separate “groups”.
They lived at Carson Metropolis & Crystal Lake.
There are several traders who trade in scrap metal since it is easily available, and has a good potential to let you earn profits.
Home windows Dwell Mail allows you to entry multiple accounts easily, together with Hotmail, Yahoo Mail premium accounts, Google’s Gmail and others.
Baldauf, Sarah. “Obtained Heartburn? A Warning About Your Proton Pump Inhibitor.” U.S.
Ding, below time strain, was in a position to only “briefly test the road”, as he described in the press conference, and as a substitute opted for 32.Kd1?
Your pediatrician or a mental well being professional might help determine any underlying conditions and supply applicable remedy.
Hopefully, this article has been informative for you and helped you choose the most effective blackwork tattoo design.
Simply stated, county civil defense and the USDA county protection boards are answerable for joint planning and post assault advice to the farm population on precautions to take to minimize radiation exposures related to farm work; county civil protection is liable for a lot of the monitoring, reporting, and evaluation of the information; and the USDA county defense board applies USDA steerage adjusted to native situations in recommending appropriate: – Care or disposition of livestock.
See the next section to explore the inventive fusion of a number of completely different kinds.
You should not make comparisons between angel investors and venture capital firms if you are considering angel investment.
Jack Chapman Lavin, Principal Ecological Officer, Bradford Metropolitan Metropolis Council.
She was born Feb.
The conference steering committee should be consulted about any adjustments to the accepted way of organizing and operating the convention.
This modeling requires an understanding of geographic distributions of people as well as an capability to calculate the probability of a natural disaster occurring.
The larger is the gap between the upper and lower price limit of the grid, the higher will be potential profits.
The ice cream distributor may be properly-capitalized either from the homeowners’ investment or from accumulated income, and may be looking to expand his markets.
You may even want to treat the powder room to a more adventurous or opulent look than in the rest of your home, indulging in ornate mirrors, lavish tile work, vividly colored wall-covering, or an unusual sink.
These events might embrace Award Ceremonies, Alumni Parties, Seller and Sales Meets, Highway shows, Training Programs, Employee Get-Together, Cocktail Parties, Teambuilding Applications for Employees, Seminars and Conferences and so forth.
Earlier than making the funding, it is very important to know about the corporate background because there are some faux corporations obtainable who cannot create a dependable title and platform for themselves, however change their firm profile to extract more money from the market.
Darth Tyranus (Rely Dooku) was a human Dark Lord of the Sith and the second apprentice of Darth Sidious, first showing in Star Wars: Episode II – Assault of the Clones.
The first is an online stock trading service that gives investors the ability to place stock trades online or by phone and receive PTI brokers鈥?assistance.
Usually, a diversified investment AIF profile is a suitable selection for funding, as adheres to the principle of danger diversification.
Mar 7-8, 2025. McKinney, TX.
Albert George Illsley. For services to the Neighborhood in Tilehurst, Studying.
Currently I have one Custom Sea Life 24 inch 65 watt sensible lamp/ half 10,000k daylight and half actinic bulb.
At Featherdale, albino wallabies are trained to stay in the shade, and the hypopigmented blue-tongued lizard (which loses skin color over time) soaks up necessary UV rays with special modulation to reduce cancer risk.
It’s difficult to use because the adhesive wants just momentary contact to type a permanent bond.
However, this result is lower by 13 from that of January 2010.
Video CD model for the Singapore market in 2001.
The devastating impacts of 10 of the worst hurricanes in U.S.
These test programs and missions revealed gaping holes in our pondering or things that we thought could be true that turned out to not be true in any respect.
Even if it hasn’t up to now, the remainder will, whether or not your interest is inventory market share costs at once or other associated angle like stock market shares, adidas historical past, market share of erp, ipod market share analyst.
Shifts may be any day of the week, at any time, as the call middle is open 24/7.
Survivors include his wife, Mrs.
This gives information about the unemployment rates and much of the economy and trading runs on unemployment rates.
In an informal poll by the Norwegian Chess Federation in 1999, this recreation was voted to be one of the best Norwegian sport.
The remainder labored in factories and mines where conditions had been a lot harsher.
The primary ingredient in Tremendous glue is cyanoacrylate (C5H5NO2, for you chemistry buffs).
Bachman Tubes (also unofficially identified as the East Ridge Tunnels), which carry Ringgold Highway (US 41/76) into the neighboring metropolis of East Ridge.
Unbeknownst to most everyone, Ford included, was that Ferrari was already in negotiations over the sale of his company to a stalwart client: the wealthy Mecom family of Texas.
In the banking sector worldwide, the Basel Accords are generally adopted by internationally active banks for tracking, reporting and exposing operational, credit and market risks.
One advantage of using Allstate is that they have a local office in each state, including Jennings, Louisiana.
This is the place the 2 PVC sleeves come into play.
He was an elder at First Presbyterian Church in Palestine and the Ralston Memorial Presbyterian Church in Houston.
You will need to compare these rates and the fees offered by these banks or currency exchange services or online providers.
The process of registering for and taking admission exams is fairly simple — there will not be numerous gimmicks or traps.
When selecting an electric typewriter, key features to think about embody the typing velocity and noise degree.
In other words, it refers to the assessment of one country’s money in relation to the money of a different country.
The match befell in Astana, Kazakhstan, from 9 April to 30 April 2023 at the St Regis Astana Resort.
MICs are updated frequently and the latest published list is available at the maintenance organization of ISO 10383 in various formats: Excel, CSV, XML and PDF.
Lots of people didn’t start learning then which created a
concertina effect where it now seems more people than ever are starting.
You have made fairly sure that you have sufficient to dwell on.
Callable CDs – CDs with a callable date might be referred to as or terminated by the issuer.
Such an approach reassures the client that he/she will call the help desk anyplace and at anytime as per his/her desires.
The St. George Defence (additionally known as the Baker’s Defence, Birmingham Defence, or Basman Counterattack) is an unorthodox chess opening for Black.
Liquidation preferences – in any liquidation event such as a merger or acquisition, the investors get their money back, often with interest and/or at a multiple, before common stock is paid any funds from liquidation.
Ermon BOYD and Mrs.
1. Bundle Your Policies: Bundling your drivers, renters, and residence insurance coverage policies with one insurer is a simple means to score a discount.
Index options enable traders to take hedged exposure to stocks of all companies, or the entire market segment, which is part of an index, as opposed to placing bets on individual company shares.
Chances are you’ll even need to deal with the powder room to a more adventurous or opulent look than in the remainder of your private home, indulging in ornate mirrors, lavish tile work, vividly colored wall-masking, or an unusual sink.
Whether it is the number of registrants, participants, or the donations collected (if it is a charity event).
Ella E. MORRISON, 75, of Star Route, Lawton, and a former longtime Fletcher resident, died at 2:15 a.m.
How do you like to travel?
Etro makes a move to make even the Pink Panther jealous, unveiling a stupendous pink jacket hugged on the waist by a black belt with a large buckle, and beneath this, a pair of trousers colored in twilight lavender.
Wednesday at the primary Presbyterian Church in Palestine with Dr.
I will see an opportunity as it develops.
In contrast, the lightly blushed moschofilero (mos-co-FEE-le-ro) is favored for dry white wines.
Behind the mass-media stereotypes, Gen-Xers were (and still are) quietly changing the world.
It is very important be prepared to deal with a medical emergency when traveling abroad for an training similar to any other person.
A modern, airy bathroom with sleek strains and city design isn’t only for big spaces.
In the money market, the excess reserves of business banks are invested in near money property (e.g., short-term payments of change), that are easily transformed into cash.
It is much easier to home practice a French bulldog puppy if he/she sleeps in a crate.
Based on GIA, the Irani Feroza gemstone is a crystalline marble formed throughout contact metamorphism.
Interesting perspective!
In 2007-08, that common was about 5 occasions as much, greater than $16,200.
Click here to obtain your FREE copy of the Gown Game!
Below are some factors that may show you how to in understanding the significance of Administration coaching packages.
These fonts look nice on a printed page, however additionally they suck down fully a lot ink.
Equally, some government bonds have been reinstated at 2.5 of face worth, to be paid after reparations have been paid.
His first season was a triumph as he answered all of the questions on how he would handle rainy Manchester compared to sunny Monaco.
This is not troublesome in nowadays as a result of there are a lot of amenities to carry out this part of Umrah, but it surely was really troublesome at the time of Hazrat Ismail (AS) when He cries for water and his mother tried to find some water.
NII is the difference between (a) interest funds the financial institution receives on excellent loans and (b) curiosity payments the bank makes to prospects on their deposits.
To encourage an energetic mood, you need to couple brilliant ambient lighting with very targeted task lighting.
A non-match, or another type of search string will take you to Wikipedia’s search results web page, where the results of your search are displayed.
Artificially low rents reduced investment in the sector, contributing to a tenure shift to owner-occupation and lower maintenance standards in the stock.
The Web’s complexity has left customers with limited choice between three large players with conflicts of interest whose positions develop extra entrenched with time.
Some types of kraft paper are very elegant and it is consumed in luxury products.
Ford’s 1958 models, like this Fairlane 500 Town Victoria hardtop sedan, had been widely thought of to be the ugliest of the decade.
Does the amount of quality and luxury match other products in this brand?
Hello there! I just would like to offer you a huge thumbs up for your great information you have right here on this post. I’ll be coming back to your website for more soon.
Once you have established a community of contacts, don’t be afraid to leverage it when looking for new opportunities.
Consumers can now use mobile phones and services like Amazon Mobile to compare a store’s prices with those of nearby competitors or online sellers.
Barry George Hook, Chief Administrative Officer, County of Avon Fireplace Brigade.
Chances are you’ll encounter further medical-related bills or need to make modifications to your house as your baby grows up.
The foremost role with the commercial property acquisition company should be to direct these buyers in creating a wise choice.
After Union army Lieutenant John Dunbar (Costner) is transferred to the army鈥檚 most distant outpost, Fort Sedgewick, he arrives to search out the put up deserted and in disrepair, however chooses to remain nonetheless.
For those who desire a sleeper import that will absolutely dominate the autocross course, yet be in a position to carry your loved ones of four to an area hockey recreation, what automotive would you be choosing?
It’s hard to find experienced people for this subject, but you sound like you know what you’re talking about! Thanks
I was very pleased to discover this site. I need to to thank you for your time due to this fantastic read!! I definitely loved every part of it and I have you bookmarked to check out new information in your site.
You’ve made some good points there. I looked on the net to learn more about the issue and found most people will go along with your views on this web site.
So what does it take to save a Television present from being canceled?
Are the plants arranged in such a method as to maximize sun publicity and water use?
I like looking through an article that can make men and women think. Also, thanks for allowing for me to comment.
Aw, this was an incredibly good post. Finding the time and actual effort to generate a great article… but what can I say… I put things off a lot and never seem to get nearly anything done.
Within the Nationwide Hockey League, the season was suspended for an indefinite amount of time, affecting the Pittsburgh Penguins and Philadelphia Flyers.
That is a great tip particularly to those new to the blogosphere. Short but very accurate information… Thank you for sharing this one. A must read post.
This could go away extra money obtainable for different areas of the provision chain, akin to packaging or transporting objects being bought.
It’s hard to come by knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks
I love it when folks get together and share opinions. Great blog, continue the good work.
We remained true to our excessive-stage objectives, but I can’t shake the feeling we might have done a better job early within the venture on the system design entrance.
Fears of the Russian-Saudi Arabian oil worth struggle caused a plunge in U.S.
Good information. Lucky me I recently found your site by accident (stumbleupon). I have saved it for later.
Good write-up. I definitely love this website. Thanks!
Balances Active Orders Withdraw Deposit TradeOgre Logout · Sign In. Search: Currency, Market, Change, Price
BPI Net Empresas bpinet é o serviço do Banco BPI que permite gerir as contas e realizar operações bancárias online, com segurança e comodidade. Saiba mais sobre as vantagens, as operações Bpi Net Empresas
Empower Your Crypto Journey
with Tangem Wallet
Greetings! Very useful advice in this particular article! It’s the little changes that produce the greatest changes. Thanks a lot for sharing!
You possibly can have a number of mates make their very own playlist so everyone will get a turn at guessing the songs.
Howdy! This post couldn’t be written any better! Looking through this article reminds me of my previous roommate! He continually kept preaching about this. I will send this article to him. Pretty sure he’s going to have a very good read. Thank you for sharing!
Buy bitcoin and exchange crypto instantly on ChangeNOW – the lowest fee crypto swap service. Enjoy fast, secure, and seamless transactions with a wide range
secux wallet
tangem wallet
TradeOgre login
noones
Markets – TradeOgre Digital Currency Exchange
TradeOgre
TradeOgre
TradeOgre
TradeOgre
TradeOgre
TradeOgre
TradeOgre
tradeogre login
tradeogre login
tradeogre login
tradeogre login
tradeogre login
tradeogre login
tradeogre login
Aw, this was a really nice post. Taking a few minutes and actual effort to create a great article… but what can I say… I procrastinate a lot and don’t manage to get nearly anything done.
Way cool! Some very valid points! I appreciate you penning this post and also the rest of the site is extremely good.
Markets – noones Digital Currency Exchange
noones
noones
noones
noones
noones
noones
noones
noones login
noones login
noones login
noones login
noones login
noones login
noones login
Markets – noones Digital Currency Exchange
noones
noones
noones
noones
noones
noones
noones
noones login
noones login
noones login
noones login
noones login
noones login
noones login
https://socialsocial.social/pin/tradeogre/
https:// tradeogre.total-blog.com/tradeogre-58734199
https://tradeogre.blog5.net/77153316/exchange-copyright
https://exchangecrypto.affiliatblogger.com/85572242/exchange-copyright
https://exchangecrypto.dbblog.net/6851587/exchangecrypto
https://exchangecrypto.fitnell.com/74298663/exchangecrypto
https://exchangecrypto.diowebhost.com/88490506/exchangecrypto
https://exchangecrypto.suomiblog.com/exchangecrypto-49141500
https://exchangecrypto.blogzet.com/exchangecrypto-48297057
https://exchangecrypto.affiliatblogger.com/85572242/exchange-copyright
https://exchangecrypto.tribunablog.com/exchangecrypto-47864289
https://exchangecrypto.shotblogs.com/exchangecrypto-47439070
https://exchangecrypto.pointblog.net/exchangecrypto-76889222
https://exchangecrypto.blogolize.com/exchangecrypto-72586907
https://exchangecrypto.over.blog/
https://socialsocial.social/pin/tradeogre/
It became an emblem of wealth, royalty, and spiritual connection.
I needed to thank you for this good read!! I absolutely enjoyed every bit of it. I’ve got you bookmarked to check out new stuff you post…
Wonderful post! We are linking to this particularly great article on our site. Keep up the good writing.
Oh my goodness! Impressive article dude! Thanks, However I am encountering difficulties with your RSS. I don’t understand the reason why I am unable to subscribe to it. Is there anybody having the same RSS issues? Anyone who knows the answer will you kindly respond? Thanx!!
I really like looking through a post that can make people think. Also, thanks for allowing for me to comment.
I’d like to thank you for the efforts you have put in penning this website. I am hoping to check out the same high-grade content from you later on as well. In truth, your creative writing abilities has motivated me to get my own, personal blog now 😉
Hello there, There’s no doubt that your site could be having browser compatibility issues. When I take a look at your site in Safari, it looks fine however when opening in IE, it’s got some overlapping issues. I simply wanted to give you a quick heads up! Aside from that, fantastic site!
Everything is very open with a clear description of the challenges. It was truly informative. Your site is very helpful. Thank you for sharing!
You are so awesome! I don’t suppose I’ve truly read anything like this before. So good to discover someone with genuine thoughts on this issue. Really.. thanks for starting this up. This site is one thing that’s needed on the internet, someone with some originality.
Hello! Do you know if they make any plugins to help with
SEO? I’m trying to get my website to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Thank you! I saw similar art here:
COD
I think this is a very valid point. I read a similar article on https://bossfun.zone that provides more context on this, and it helped me think about it from a different angle.
I enjoy reading through an article that can make people think. Also, thanks for permitting me to comment.
I used to be able to find good information from your blog articles.
Kaufman, including that a number of different gluten-free foods are processed to the hilt, and truly are nutrient-poor, in contrast to quinoa.
Some folks say that worrying about knowledge security is a moot level.
Which type of footwear finest matches your character?
The ensemble is anticipated to fetch a minimal of $7,000 (£4,800), one thing of a bargain price as it initially set the singer back $40,000 (£27,700).
Reed, Brad. “LTE vs. WiMAX.” Community World.
There might be no learning below fear.
I am extremely impressed along with your writing skills as smartly as
with the format in your weblog. Is this a paid theme or did you customize it your self?
Either way stay up the nice high quality writing, it is uncommon to look a nice blog
like this one today. Snipfeed!
Good information. Lucky me I discovered your website by accident (stumbleupon). I have book marked it for later.
Good article! We will be linking to this great content on our website. Keep up the great writing.
Oh my goodness! Impressive article dude! Thank you, However I am encountering difficulties with your RSS. I don’t know why I am unable to subscribe to it. Is there anybody having the same RSS issues? Anyone who knows the answer can you kindly respond? Thanks!!
On July 1, just as the ship was about to sail, the Portol脿/Serra get together arrived in San Diego in good health, with 163 mules loaded with supplies.
It strips away heavy buildup (from conditioners, merchandise, whatever) that weighs hair down, making it look lifeless and flat.
Inside the layer, air molecules which are trapped cannot get out, despite the fact that they’re pushing towards the water.
The company provides attention-grabbing provides and tempting markets to landowners wanting for brief and long time rentals.
The first £1million of combined enterprise and agricultural assets will proceed to draw no inheritance tax.
I must thank you for the efforts you’ve put in writing this blog. I’m hoping to check out the same high-grade blog posts by you later on as well. In fact, your creative writing abilities has encouraged me to get my own, personal site now 😉
This is a topic that’s close to my heart… Thank you! Where are your contact details though?
Hedging additionally will increase liquidity in the marketplace for numerous asset courses.
An intriguing discussion is definitely worth comment. There’s no doubt that that you need to publish more on this topic, it might not be a taboo matter but generally people don’t speak about these issues. To the next! Best wishes!
Yes, I agree with this view completely. There’s an insightful post on hitclub that covers this very subject, and I think it provides a solid argument to support your point.
I completely agree with you. This viewpoint is one I’ve encountered in several articles on https://bossfun.zone, which provide thoughtful analysis on the subject.
Proper management, planning and implementation are necessary to prosper a occasion.
Corporations will then discover many of the operations enacted in the business are directly transparent and in appropriate order.
Joseph William Deegan, CVO, lately Commissioner of Police, Uganda, now Deputy Inspector-General of Colonial Police.
The Forex exchange market is an over-the counter market with no central trade policies.
The solar’s rays are surprisingly powerful, and a few of its most highly effective rays — referred to as ultraviolet (UV) rays — are actually invisible.
Great info. Lucky me I discovered your site by chance (stumbleupon). I’ve bookmarked it for later.
There’s certainly a great deal to learn about this subject. I really like all the points you made.
By December 24, the situation of the severely burned Leginos started to improve.
It’s hard to come by experienced people about this subject, but you sound like you know what you’re talking about! Thanks
In accordance with World Population Assessment, the nation as an entire has a population density of 93.29 folks per sq.
You are so awesome! I do not think I’ve truly read through anything like this before. So great to discover somebody with a few unique thoughts on this subject. Really.. many thanks for starting this up. This site is one thing that’s needed on the internet, someone with some originality.
When I originally commented I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve four emails with the same comment. Is there an easy method you are able to remove me from that service? Thanks.
Pretty! This was an extremely wonderful post. Thanks for supplying these details.
Hello! I know this is kind of off-topic but I had to ask.
Does building a well-established website such as yours take a massive amount work?
I am completely new to operating a blog however I do write
in my journal daily. I’d like to start a blog so I can easily share my own experience and views online.
Please let me know if you have any suggestions
or tips for new aspiring blog owners. Thankyou!
An outstanding share! I have just forwarded this onto a colleague who had been conducting a little homework on this. And he actually ordered me dinner simply because I found it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanx for spending time to talk about this matter here on your site.
High on risk and high on return are Equity funds.
In accordance to numerous research and analysis finished on this domain it has been projected that the future of the financial boom sample in India which is clearly visible lies on the character of its manufacturing sector which includes the Stainless Steel manufacturing firm.
Through the opening press convention, Anand revealed his new seconds to be Krishnan Sasikiran, Sandipan Chanda and Peter Leko.
Center the rooster as a stand-alone design on a chair seat or serving tray.
Often they went over to the network broadcast at various times of the night, and often they showed some community items later than when the English areas noticed them.
Fish and wildlife are weak to the oil spill ensuing from the explosion and sinking of the Deepwater Horizon oil rig.
Analysis in synthetic photosynthesis is choosing up steam, but it will not be leaving the lab any time quickly.
There’s certainly a great deal to know about this subject. I love all the points you’ve made.
I am really inspired together with your writing abilities as neatly
as with the structure in your weblog. Is this a paid theme
or did you customize it your self? Anyway stay
up the excellent quality writing, it is uncommon to
see a great blog like this one nowadays.
Beacons AI!
An intriguing discussion is definitely worth comment. I do think that you ought to publish more on this issue, it might not be a taboo subject but generally people don’t discuss these topics. To the next! Many thanks.
I think this point is spot-on. I’ve read something quite similar on https://hdbet.deal, and it helped me to expand my understanding of the subject even further.
Very good post! We are linking to this particularly great article on our site. Keep up the great writing.
I’m impressed, I must say. Seldom do I come across a blog that’s both equally educative and amusing, and let me tell you, you’ve hit the nail on the head. The problem is something which too few people are speaking intelligently about. I’m very happy that I stumbled across this during my search for something relating to this.
I totally agree with this statement. It mirrors a post I read on For88, where they provided a lot of useful information to support this viewpoint.
I am extremely inspired together with your writing skills and also with the layout to your blog. Is this a paid subject matter or did you modify it your self? Anyway keep up the excellent quality writing, it’s rare to peer a great blog like this one these days. I like nurseseducator.com ! It is my: Instagram Auto follow
As absolutely as the crocuses bloom and other people begin sneezing, the rains will come.
You’re absolutely right, I completely agree with your perspective. I found similar discussions on V8club, which provided a lot of insight into this topic.
Hessian troops briefly occupied Bordentown in 1776 as part of the brand new York and New Jersey marketing campaign earlier than leaving to have interaction in the Battle of Iron Works Hill on December 23.
That is a great tip especially to those fresh to the blogosphere. Brief but very accurate information… Appreciate your sharing this one. A must read article.
I blog often and I really thank you for your content. The article has really peaked my interest. I am going to take a note of your website and keep checking for new details about once a week. I subscribed to your RSS feed as well.
During her profession, she coined two maneuvers still used by gymnasts at this time: the Comaneci salto and the Comaneci dismount.
The main industries are agro-processing (like beer manufacturing and sugar cane crushing).
Helpful content!
This website was… how do I say it? Relevant!! Finally I have found something that helped me. Many thanks!
Well written, thanks!
Saved as a favorite, I really like your web site.
After looking at a few of the articles on your website, I seriously appreciate your technique of blogging. I added it to my bookmark webpage list and will be checking back in the near future. Take a look at my website too and tell me your opinion.
bookmarked!!, I love your blog.
This is gold, thanks!
Aw, this was a very good post. Taking a few minutes and actual effort to create a top notch article… but what can I say… I put things off a whole lot and don’t seem to get anything done.
Easy to digest.
Just wow.
I could not refrain from commenting. Well written.
I fully agree with this view, and I think it’s an important one to highlight. I’ve seen similar opinions shared on https://zo10win.com/, which provide some really valuable insights into this topic.
Love how actionable this is.
Absolutely, this perspective makes a lot of sense. It’s similar to what I read a while ago on Tin88, and it helped me understand the issue much better.