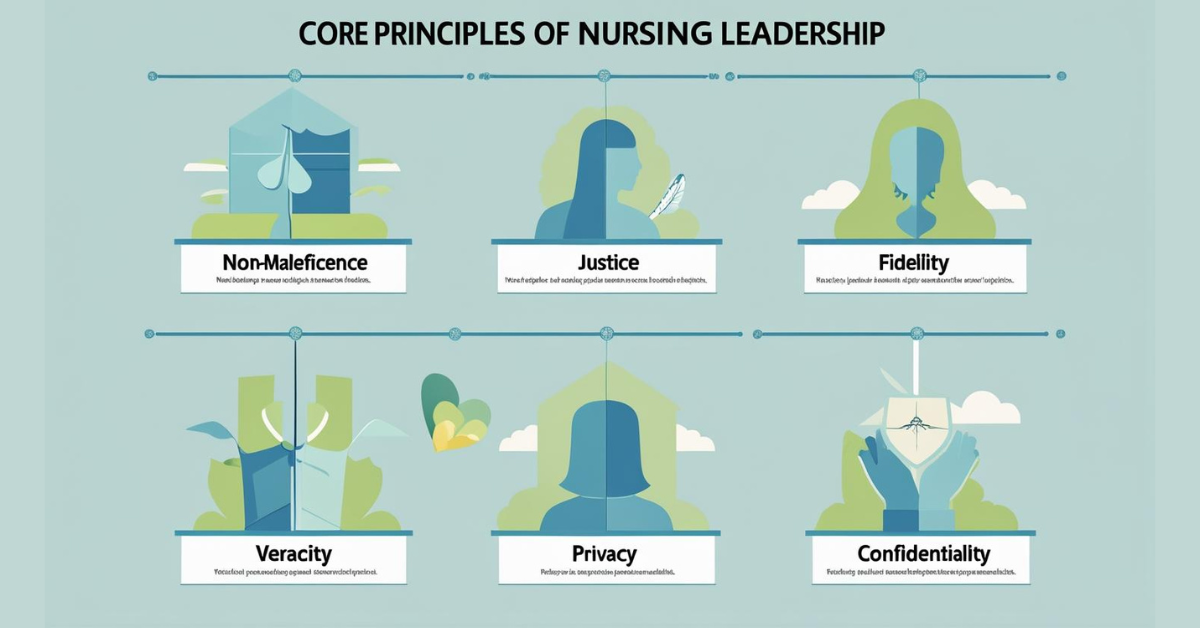
What is Non-Maleficence Justice Fidelity Veracity Privacy and Confidentiality In Nursing Practices for Leadership. In nursing practice, non-maleficence, justice, fidelity, truthfulness, privacy, and confidentiality are fundamental ethical principles that guide leadership. These principles ensure patient well-being, fair treatment, trusting relationships, honesty, and the protection of sensitive information.
The Non-Maleficence Justice Fidelity Veracity Privacy and Confidentiality In Nursing Practices for Leadership
Although there are many ethical principles that guide nursing practice, basic ethical principles include respect for autonomy and self-determination, beneficence (doing good), non-maleficence (doing no harm), justice (fairness), fidelity (keeping promises), and veracity (telling the truth).
1. Non-maleficence: This principle emphasizes the need to avoid harm to patients, both intentional and unintentional. Nurse leaders must ensure that practices minimize risks to patients, healthcare professionals, and the organization. Some examples include implementing safety protocols, preventing medication errors, and implementing appropriate infection control measures.
2. Equity: Equity in nursing refers to fairness and the equitable distribution of care. Nurse leaders must ensure that all patients receive the same care, regardless of their background, socioeconomic status, or other factors. This includes impartial decision-making, prioritizing patient care based on their needs, and advocating for equitable access to healthcare resources.
3. Fidelity: Fidelity means keeping promises and being faithful to commitments to patients. Nurse managers must demonstrate trustworthiness and establish close relationships with their teams and patients. Some examples include fulfilling specific care commitments, maintaining confidentiality, and honoring requests.
4. Veracity: Veracity is the principle of truthfulness and honesty in communication with patients. Nurse managers must ensure that patients receive accurate and complete information about their condition, treatment options, and prognosis. This includes openness and honesty, even when the truth is difficult for the patient to accept.
5. Privacy: Privacy in nursing refers to the patient’s right to control access to their personal data. Nurse managers must ensure that patient information is shared only with those directly involved in their care and that appropriate security measures are implemented to protect patient confidentiality.
6. Confidentiality: Confidentiality extends data protection by requiring nurses to protect sensitive patient information from unauthorized disclosure. Nurse managers must establish clear policies and protocols to ensure the responsible handling of patient information and the protection of patient privacy.
Role of Nurse Managers
Set the tone
Nurse managers must model ethical behavior and create a culture of ethical action within their teams.
Provide leadership and support
Nurse managers must advise their teams on ethical decisions and support them through ethical dilemmas.
Promote ethical awareness
Nurse managers must educate their teams on ethical principles and ensure they understand their responsibility to adhere to ethical standards.
Addressing Ethical Concerns
Nurse managers must be prepared to address ethical concerns and conflicts within their teams and ensure they are resolved fairly and ethically.
Non-Maleficence
The principle of non-maleficence refers to the moral obligation to do no harm or injury to another person. Nurses honor the principle of non-maleficence by following standards of care and implementing best practices. Non-maleficence also involves an obligation to avoid imposing risks of harm to another and includes moral rules such as the following (Beauchamp & Childress, 2009, p. 153):
- Do not kill.
- Do not cause pain or suffering.
- Do not incapacitate.
- Do not cause offense.
- Do not deprive others of goods of life.
Non-maleficence differs from beneficence in that non-maleficence morally prohibits people from causing harm to anyone; beneficence is failing to help or benefit another, but it is not always considered immoral (Beauchamp & Childress, 2009). Some situations result in a conflict between beneficence and non-maleficence and presenting challenges for nurses and other health-care professionals. A common example is the administration of chemotherapy.
Chemotherapeutic agents destroy cancer cells but also healthy cells and have extremely uncomfortable side effects. When providing chemotherapy, nurses violate the principle of non-maleficence in the short term to produce a good outcome or benefit the patient in the long term. Related to the principles of beneficence and non-maleficence is paternalism, which is “the intentional overriding of one person’s preferences or actions by another person” (Beauchamp & Childress, 2009, p. 208) or, in the health-care world, con trolling a patient’s choices.
Many nurses often justify paternalism in the name of beneficence and non-maleficence. Many times a nurse, because of his or her knowledge, education, and experience, may believe that he or she knows what is best for the patient and act accordingly regardless of the patient’s wishes. This interferes with the patient’s autonomy and right to self-determination.
Nurses must be able to differentiate between controlling patient choices, or paternalism, and assisting patients in making informed choices, or respecting autonomy. For example, when a nurse decides not to tell a patient that his or her temperature is elevated or his or her heart rate is irregular because the nurse believes that the news will upset the patient, that nurse is acting in a paternalistic manner. The nurse is deciding for the patient whether he or she should be told this information.
Justice
The principle of justice refers to the obligation of nurses to provide fair, equitable, and appropriate treatment to all patients based on their needs and without prejudice. Justice is about treating everyone equally and fairly and giving people what they deserve. Nurses apply the principle of justice when they deliver care to patients without bias.
However, the principle of justice can be very complicated, especially when considering inequalities in access to health care and health insurance. Nurse leaders and managers apply justice professionally when they promote giving staff members adequate compensation commensurate with education, experience, and responsibilities (ANA, 2016).
Fidelity
The principle of fidelity refers to being faithful or loyal by keeping promises to others. Fidelity is fundamental for the nurse-patient relationship and requires nurses to be loyal, truthful, fair, and advocates for patients. When nurses receive their nursing license, they accept the mandate to practice nursing within established scope and standards of practice, which includes keeping promises to patients (Burkhardt & Nathaniel, 2008).
Nurse leaders and managers apply fidelity professionally when they keep promises to staff by maintaining a culture of safety and a healthy work environment, one that is empowering and satisfying. (A healthy work environment is discussed further ) Nurse leaders and managers must be mindful of the health and safety of both patients and their staff members.
Veracity
The principle of veracity, which is connected to autonomy and fidelity, is the notion that patients have a right to truthful information. When nurses enter the nurse patient relationship, they must speak truthfully and not be deceptive.
Overall, society trusts health-care professionals; moreover, nurses consistently rank number one by the public regarding professional honesty and ethical standards (Riffken, 2014). Nurse leaders and managers apply the principle of veracity professionally when they are truthful with employees and avoid intentionally deceiving or misleading staff.
Privacy
The principle of privacy refers to a person’s right to have control over access to his or her personal information. Privacy is not just an ethical principle but also a legal right and is protected by the Health Insurance Portability and Accountability Act (HIPAA), which is discussed later in this topic. Patients confide in nurses and trust them with personal information.
Nurses, in turn, must respect patients’ privacy and discuss patient information only with other health-care professionals and only if they have a need to know. Nurse leaders and managers promote patient privacy when they create an environment that allows for physical and auditory privacy for discussion of patient information and establish policies and procedures that protect patient confidentiality (ANA, 2015a). Nurse leaders and managers show respect for employee privacy by keeping an employee’s religious beliefs and lifestyle choices private.
Confidentiality
Patients have little or no choice to share private information with nurses and other members of the health-care team. The principle of confidentiality means preventing disclosure of private information shared between a patient and the health-care team. Once a patient shares personal information, the nurse can use that information only as authorized by the patient. Nurses are required to maintain confidentiality of all patient information.
Although confidentiality is similar to privacy, there is a difference between the two: An infringement of a person’s right to confidentiality occurs only if the person (or institution) to whom the information was disclosed in confidence fails to protect the information or deliberately discloses it to someone without first-party consent. By contrast, a person who, without authorization, enters a hospital record room or computer database violates rights of privacy, although he or she may also obtain confidential information.
Only the person or institution who obtains information in a confidential relationship can be charged with violating the rights of confidentiality (Beauchamp & Childress, 2009, pp. 302–303). Nurses at all levels have a duty to maintain confidentiality of all patient information, both personal and clinical, in the work setting and off duty in all venues including social media or any other means of communication (ANA, 2015a, p.9).
Nurse leaders and managers provide employees confidentiality by securing their personal information such as Social Security numbers and medical information. Only staff members who have a legitimate need within the performance of their job duties should have access to employee personal information.
Read More:
https://nurseseducator.com/didactic-and-dialectic-teaching-rationale-for-team-based-learning/
https://nurseseducator.com/high-fidelity-simulation-use-in-nursing-education/
First NCLEX Exam Center In Pakistan From Lahore (Mall of Lahore) to the Global Nursing
Categories of Journals: W, X, Y and Z Category Journal In Nursing Education
AI in Healthcare Content Creation: A Double-Edged Sword and Scary
Social Links:
https://www.facebook.com/nurseseducator/
https://www.instagram.com/nurseseducator/
https://www.pinterest.com/NursesEducator/
https://www.linkedin.com/in/nurseseducator/
https://www.researchgate.net/profile/Afza-Lal-Din
https://scholar.google.com/citations?hl=en&user=F0XY9vQAAAAJ
Thank you so much for giving everyone an exceptionally memorable possiblity to check tips from this blog. It is always very cool and also stuffed with a lot of fun for me and my office friends to visit your web site on the least three times every week to study the newest things you have. And definitely, I’m just at all times fulfilled with all the magnificent solutions you give. Some 4 areas in this post are essentially the most impressive I’ve had.
Hello there, You’ve done an excellent job. I will certainly digg it and personally suggest to my friends. I am sure they will be benefited from this web site.
I like foregathering utile information , this post has got me even more info! .