The Modes of Mechanical Ventilation Mechanical ventilation is a life-saving intervention employed in various clinical settings to assist or replace spontaneous breathing in patients who are unable to breathe adequately on their own.
Understanding the modes of mechanical ventilation is essential for healthcare providers, as it influences patient outcomes and facilitates effective respiratory management. This comprehensive guide explores the modern approaches to modes of mechanical ventilation, emphasizing the distinctions between volume-controlled and pressure-controlled modes, as well as advanced modes and strategies.
The Modern Approach to Mechanical Ventilation
Classifications of Ventilatory Modes
Traditionally, mechanical ventilation modes were categorized into pressure-controlled and volume-controlled modes. However, a more contemporary classification focuses on three critical characteristics:
- Trigger: The mechanism that initiates the breath (e.g., flow or pressure).
- Limit: The factor that determines the size of the breath (e.g., pressure or volume).
- Cycle: The event that terminates the breath.
This framework allows for a more nuanced understanding of how different modes function, especially as technology advances and blurs the lines between traditional classifications.
Key Terminologies
- Volume-Controlled Modes: These modes deliver a set volume of air with each breath, ensuring that the patient receives consistent tidal volumes regardless of lung mechanics.
- Pressure-Controlled Modes: In these modes, a set pressure is delivered with each breath, allowing for varying tidal volumes depending on the compliance and resistance of the respiratory system.
Volume Modes of Mechanical Ventilation
Assist-Control Ventilation (ACV)
Also known as Continuous Mandatory Ventilation (CMV), ACV provides a predetermined tidal volume for each mechanical breath. This mode can lead to hyperinflation if the inspiratory-expiratory (I) ratio is less than 1:2, particularly in patients with rapid respiratory rates. While ACV ensures consistent ventilation, it does not eliminate the work of breathing, as the diaphragm may still be actively involved.
Synchronized Intermittent-Mandatory Ventilation (SIMV)
SIMV allows for a combination of mandatory and spontaneous breaths, with mandatory breaths synchronized to the patient’s spontaneous efforts. This mode reduces the risk of hyperinflation and respiratory alkalosis associated with ACV, but it may increase the work of breathing and potentially lower cardiac output. Nursing considerations include monitoring the patient’s respiratory rate and effort to determine the appropriateness of SIMV versus ACV.
https://www.instagram.com/p/DSWjxEzCmeP/?igsh=cDF5OTg4YXo5YTV3
Pressure Modes of Mechanical Ventilation
Pressure-Controlled Ventilation (PCV)
PCV is characterized by a set pressure delivered during each breath, with the primary goal of minimizing barotrauma. However, this mode does not guarantee a specific tidal volume, making it more suitable for patients with neuromuscular diseases but otherwise normal lung mechanics.
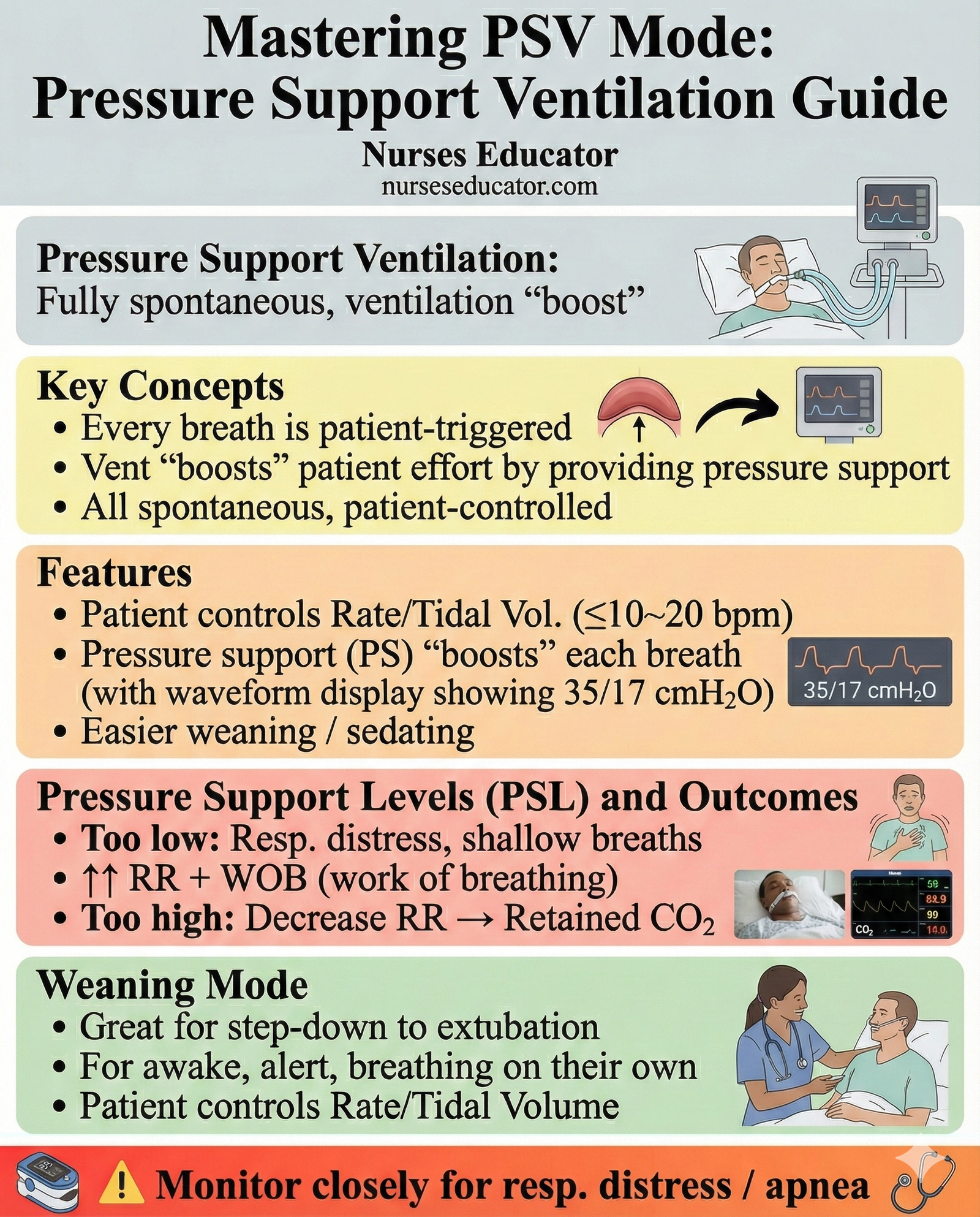
Pressure Support Ventilation (PSV)
PSV allows patients to initiate their own breaths, with the ventilator providing pressure support to assist with inhalation. This mode can help patients overcome the resistance of the ventilator tubing and may be beneficial during weaning from mechanical ventilation.
Pressure Controlled Inverse Ratio Ventilation (PCIRV)
In PCIRV, the inspiratory time is prolonged, which may improve oxygenation but carries risks of auto-PEEP and hemodynamic instability. This mode is typically used for patients with severe respiratory failure, where maintaining adequate oxygenation is critical.
Airway Pressure Release Ventilation (APRV)
APRV is a unique mode that combines continuous positive airway pressure (CPAP) with intermittent pressure releases. This mode allows for spontaneous breathing at both high and low pressures, promoting lung recruitment while minimizing the risk of barotrauma.
Advanced Ventilatory Modes
Pressure Regulated Volume Control (PRVC)
PRVC combines the principles of volume-targeted ventilation with pressure control. It provides a set tidal volume while adjusting the pressure as needed based on the patient’s respiratory mechanics.
Proportional Assist Ventilation (PAV)
PAV allows for variable levels of support based on the patient’s efforts, enhancing synchrony and comfort. This mode uses a positive feedback loop that requires real-time calculations of the patient’s respiratory resistance and compliance.
Neurally Adjusted Ventilatory Assist (NAVA)
NAVA is a mode that utilizes the electrical activity of the diaphragm to trigger ventilation, promoting patient-ventilator synchrony and comfort. This innovative approach enhances the ability to tailor ventilation to the patient’s needs.
Additional Ventilation Strategies
Positive End-Expiratory Pressure (PEEP)
PEEP is an important strategy used to prevent alveolar collapse at the end of expiration. While it increases mean airway pressure, it can also affect cardiac output and should be monitored closely in patients with hemodynamic instability.
Continuous Positive Airway Pressure (CPAP)
CPAP provides continuous pressure to maintain open airways, beneficial in conditions like obstructive sleep apnea and acute respiratory distress syndrome (ARDS). This mode can improve oxygenation and is often used in non-invasive ventilation settings.
Inverse Ratio Ventilation (IRV)
IRV is a strategy that prolongs inspiratory time, which can be useful in patients with ARDS. By increasing the mean airway pressure, IRV may enhance oxygenation; however, it may also compromise hemodynamics.
High-Frequency Oscillatory Ventilation (HFOV)
HFOV delivers small tidal volumes at very high frequencies, which can help prevent ventilator-induced lung injury while providing adequate gas exchange. This mode is often used in pediatric patients or those with severe ARDS.
Conclusion
Mechanical ventilation is an essential aspect of critical care that requires a comprehensive understanding of various modes and strategies. The selection of an appropriate mode is influenced by the patient’s underlying condition, respiratory mechanics, and overall goals of treatment. Continuous education and training in the use of mechanical ventilation are vital for healthcare providers to ensure optimal patient outcomes and minimize complications. As technology advances, the field of mechanical ventilation will continue to evolve, necessitating ongoing research and adaptation in clinical practice.
Read More:
https://nurseseducator.com/didactic-and-dialectic-teaching-rationale-for-team-based-learning/
https://nurseseducator.com/high-fidelity-simulation-use-in-nursing-education/
First NCLEX Exam Center In Pakistan From Lahore (Mall of Lahore) to the Global Nursing
Categories of Journals: W, X, Y and Z Category Journal In Nursing Education
AI in Healthcare Content Creation: A Double-Edged Sword and Scary
Social Links:
https://www.facebook.com/nurseseducator/
https://www.instagram.com/nurseseducator/

Howdy! This is my first comment here soo I just wanted to give a quick shout out and tell youu I really
enjoy reading your blog posts. Can you recommend any other
blogs/websites/forums that go over the same subjects? Appreciate it! https://Glassi-Greyhounds.Mystrikingly.com/