Master Autism in the ER: 7 Evidence-Based Techniques for Assessing Pain in Non-Verbal Adults (2026 Nurse’s Guide). Ache evaluation for non-verbal autistic adults in emergency settings. Discover 7 verified techniques, behavioral indicators, and communique techniques nurses want in 2026.
7 Evidence-Based Techniques for Assessing Pain in Non-Verbal Adults (2026 Nurse’s Guide): Autism in the ER
Introduction
Emergency departments come upon about 2.3 million visits yearly from adults with autism spectrum sickness consistent with the Agency for Healthcare Research and Quality 2025 National Emergency Department Sample, with thirty- percentage of those sufferers demonstrating minimum or no verbal communique abilities. Pain evaluation in non-verbal autistic adults represents one of the maximum hard medical eventuality’s emergency nurses faces, as conventional self-document ache scales show completely insufficient at the same time as unrecognized ache ends in behavioral escalation, diagnostic delays, and insufficient analgesia provision.
Research posted with inside the Annals of Emergency Medicine demonstrates that non-verbal autistic sufferers get hold of ache medicine forty-seven percentage much less often than neurotypical sufferers imparting with equal damage severity, reflecting evaluation screw ups in place of decreased ache experiences.
The Gate Control Theory of Pain advanced with the aid of using Ronald Melzack and Patrick Wall emphasizes that ache represents a complicated neurological revel in related to sensory, emotional, and cognitive components, all of which happen in another way in autistic people whose sensory processing, emotional expression, and communique styles diverge extensively from neurotypical shows requiring evaluation change.
Understanding Pain Experience and Expression in Autistic Adults
Autism spectrum sickness essentially alters how people perceive, method, and talk ache sensations, developing profound evaluation demanding situations in emergency settings in which speedy assessment drives remedy decisions. Neurological variations in sensory integration suggest autistic adults may also reveal hyposensitivity to sure aches at the same time as experiencing hypersensitive reaction to others, once occasionallyhe identical individual.
The sensory processing versions documented substantially in occupational remedy literature provide an explanation for why a few autistic sufferers seem detached to accidents inflicting excessive misery in neurotypical people at the same time as concurrently experiencing overwhelming ache from minor tactile stimuli, vivid lights, or environmental sounds.
Interception, the neurological method allowing cognizance of inner frame states such as ache, hunger, and fatigue, regularly features atypically in autistic people in accordance to analyze in Neuroscience and Bio behavioral Reviews. Reduced interceptive cognizance approach a few autistic adults cannot as it should be discover ache sources, describe sensation qualities, or differentiate ache depth tiers even if owning verbal abilities. This neurological distinction represents real physiological variant in place of willful noncompliance or highbrow difficulty requiring clinician reputation and accommodation.
Pain communique in non-verbal autistic adults does not often resemble traditional expressions such as grimacing, groaning, or verbally soliciting for relief. Instead, ache manifestations may also encompass stimming intensification, self-injurious behaviors, aggression in the direction of others, social withdrawal, or reputedly unrelated behavioral modifications that emergency groups of workers misread as psychiatric symptoms, behavioral problems, or autism-associated traits in place of spotting them as ache indicators.
The biopsychosocial version of ache articulated with the aid of using George Engel emphasizes that ache evaluation needs to include biological, psychological, and social contextual factors, all requiring change whilst carried out to autistic populations.
Seven Evidence-Based Techniques for Non-Verbal Pain Assessment
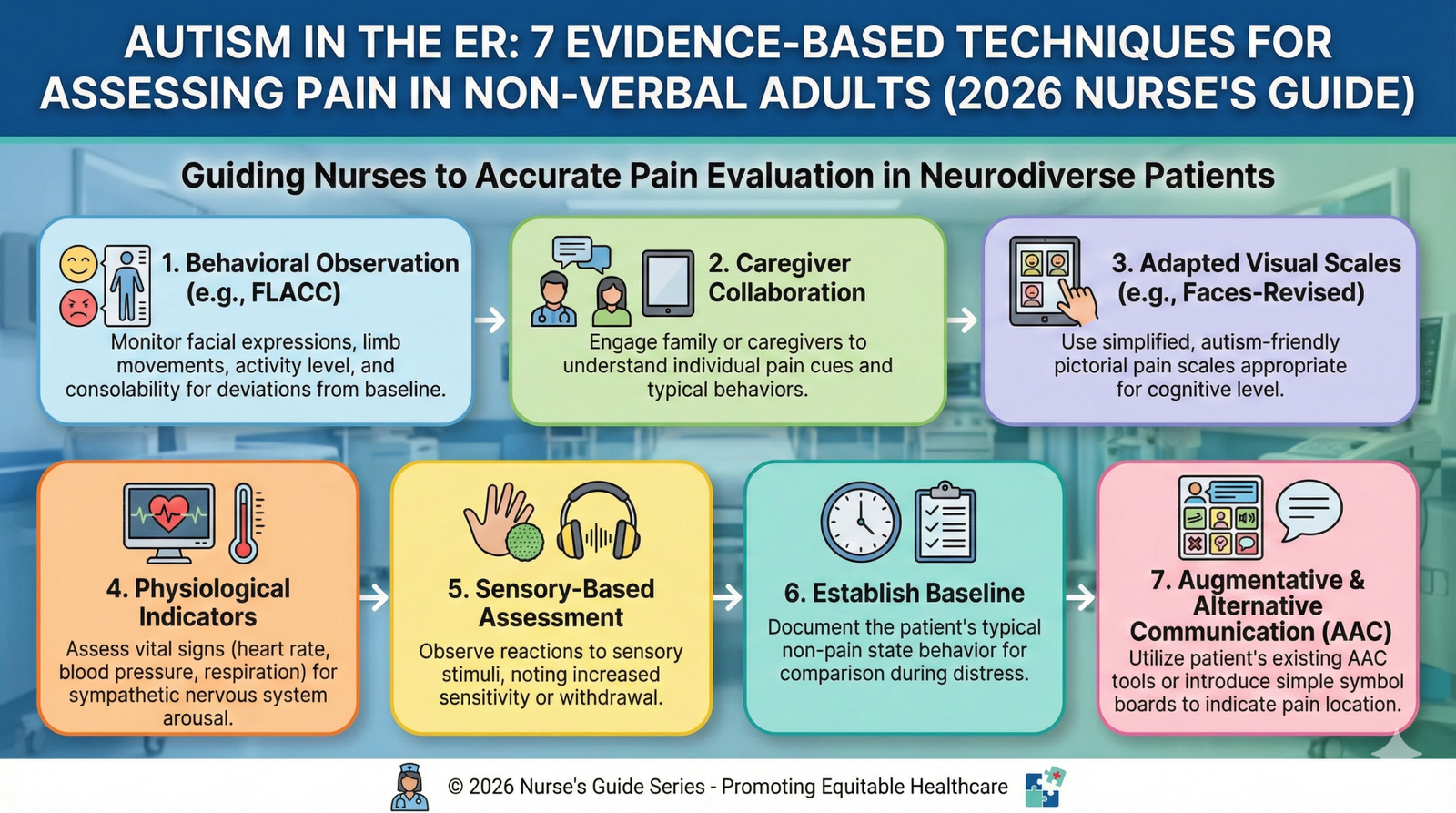
Utilize Validated Observational Pain Assessment Tools Adapted for Autism
Several ache evaluation devices reveal validity for non-verbal populations whilst well administered via way of means of skilled observers acquainted with person baseline behaviors. The revised Face, Legs, Activity, Cry, Consolability scale tailored for cognitive impairment evaluates 5 behavioral domain names on 0-to- factor scales, generating composite rankings starting from 0 to 10 that correlate with ache severity. Emergency nurses must verify facial expressions noting forehead furrowing, eye squeezing, or grimacing; leg positioning inclusive of restlessness, tension, or shielding guarding; pastime degrees and frame movements; vocalization styles; and Consolability responses to consolation measures.
The Non-Communicating Children`s Pain Checklist – Revised, notwithstanding its pediatric origins, demonstrates application for non-verbal autistic adults whilst observers account for developmental as opposed to chronological age appropriateness. This complete device evaluates vocal responses, social-character modifications, facial expressions, pastime styles, frame language, physiological indicators, and eating-napping disruptions throughout thirty observable behaviors. Research in Pain Management Nursing validates that methodical observational device utility considerably improves ache reputation accuracy in comparison to unstructured medical impression, although emergency nurses should get hold of unique schooling as opposed to assuming intuitive competency.
Withouttical Care Pain Obreactions, at the beginning advanced for robotically ventilated extensive care sufferers, assesses facial expressions, frame movements, muscle tension, and ventilator compliance generating rankings among 0 and 8. This device’s simplicity and attention on observable behaviors without requiring verbal reaction makes it specifically relevant to emergency branch autistic sufferers experiencing acute ache. However, all standardized equipment reveals boundaries whilst autistic individuals’ baseline shows encompass behaviors the devices categorize as ache indicators, necessitating individualized baseline status quo on every occasion possible.
Establish Individual Behavioral Baselines Through Caregiver Collaboration
Family members, residential aid staff, and different caregivers accompanying autistic sufferers own worthwhile information concerning person baseline behaviors, traditional ache expressions, powerful consolation strategies, and verbal exchange styles that emergency employee can’t figure thru short medical encounters. The Partnered Care version acknowledges caregiver information as complementary to nursing information as opposed to subordinate to expert evaluation, growing collaborative relationships that considerably enhance medical outcomes.
Emergency nurses must systematically elicit caregiver enter the use of based questions addressing how the person normally expresses ache, what behavioral modifications induced emergency branch presentation, what consolation measures show powerful, and what sensory sensitivities require accommodation.
Creating short caregiver questionnaires finished all through triage captures important statistics earlier than remedy crew fragmentation and emergency branch chaos disperses those informed partners. Questions must deal with baseline verbal exchange methods, traditional stimming behaviors, regarded ache expressions, powerful calming strategies, sensory choices and aversions, medicinal drug sensitivities, and any increase care making plans documentation. The Emergency Information Form advanced via way of means of the American College of Emergency Physicians and American Academy of Pediatrics offers frameworks adaptable for autistic grownup populations making sure systematic statistics capture.
Video recordings of baseline behaviors supplied through caregivers provide effective contrast equipment allowing emergency workforce to discover deviations indicating ache or misery. Some households preserve phone films documenting their cherished one’s standard presentation, satisfied effect, and snug behaviors that assess sharply with cutting-edge emergency branch presentation, imparting goal proof of sizable alternate even if numerical ache scales show inapplicable.
Implement Systematic Physiological Monitoring and Vital Sign Trending
Physiological parameters inclusive of coronary heart rate, blood strain, respiration rate, oxygen saturation, and pupillary responses offer goal ache signs supplementing behavioral observations, although emergency nurses should understand that a few autistic people show abnormal autonomic responses to ache. Tachycardia, hypertension, tachypnea, and diaphoresis constitute conventional sympathetic fearful machine activation markers suggesting ache or misery, although anxiety, sensory overload, and environmental pressure produce same physiological modifications complicating interpretation in emergency settings inherently offering these kinds of elements.
Serial critical signal measurements figuring out traits show greater preciousness than remote readings, such as innovative tachycardia or blood strain elevation following precise interventions or role modifications indicates ache exacerbation whilst physiological normalization following analgesia management presents retrospective validation of ache presence. The trouble includes time constraints in emergency settings in which remedy choices cannot look forward to enormous tracking periods, although nurses need to maximize to be had statistics through making sure constant critical signal evaluation periods and cautious trending documentation.
Pupillary dilation represents an autonomic ache reaction much less difficult to aware manage than behavioral expressions, although scholar evaluation in autistic sufferers calls for accounting for mydriatic medicinal drug effects, neurological conditions, and baseline variations. Some studies indicate pupillometry the usage of computerized infrared gadgets presents greater touchy ache detection than traditional evaluation methods, although those technologies stay unavailable in maximum emergency departments restricting cutting-edge medical applicability.
Conduct Methodical Physical Examination with Trauma-Informed Approaches
Systematic bodily exam figuring out anatomical ache reassets proves critical while sufferers cannot verbally file symptom vicinity or characteristics, although exam approaches themselves may also purpose extra misery for autistic people touchy to sudden touch, role modifications, and social interaction. Trauma-knowledgeable exam techniques decrease useless misery whilst maximizing diagnostic data through improving caution earlier than every touch, permitting sufferers to peer drawing close hands, the usage of organization strain in place of mild stroking that can sense unpleasantness, and intending methodically from much less touchy to greater touchy regions.
Visual exams for injuries, asymmetry, swelling, discoloration, or deformity need to precede palpation each time possible, as a few findings show obvious without requiring painful manipulation. When palpation becomes necessary, emergency nurses need to study facial expressions, frame tension, protecting movements, and vocalization modifications for the duration of exam, noting which anatomical regions produce most powerful reactions. Starting exams in regions, at least probable to harbor pathology establishes baseline responses facilitating contrast while inspecting probably injured regions.
Some autistic adults tolerate self-directed exams higher than provider-managed evaluation, permitting sufferers to press their very own stomach or pass their very own extremities whilst nurses’ study for ache behaviors. This technique respects affected person autonomy whilst preserving exam rigor, although it calls for time and persistence that emergency branch workflows hardly ever accommodate notwithstanding ability diagnostic value.
Apply Analgesic Trials as Diagnostic and Therapeutic Interventions
When ache presence stays unsure in spite of observational evaluation and exam findings, empiric analgesia management observed through behavioral reassessment affords each diagnostic records and healing benefit. If behavioral agitation, crucial signal abnormalities, or misery markers appreciably enhance following ache remedy, retrospective ache analysis will become obtrusive despite the fact that potential identity proved elusive. This technique aligns with emergency medicinal drug standards emphasizing fast symptom remedy even as pursuing definitive analysis, although suitable remedy choice and dosing call for cautious consideration.
Starting with non-opioid analgesics consisting of acetaminophen or ibuprofen minimizes detrimental impact dangers even as supplying good enough remedy for mild-to-slight ache, with remedy reaction commentary over thirty to sixty mins earlier than escalating to more potent agents. Autistic people regularly display heightened remedy sensitivity requiring dose discounts from preferred protocols, although a few sufferers metabolize medicines swiftly necessitating better doses or shorter dosing intervals. Caregiver enters concerning preceding remedy stories proves beneficial for secure prescribing.
Topical anesthetics, ice application, and positioning adjustments constitute extra analgesic techniques generating observable responses whilst ache motivates contemporary presentation. The multimodal analgesia technique combining pharmacological and non-pharmacological interventions frequently proves handiest even as minimizing person remedy doses and related facet effects.
Recognize Autism-Specific Pain Behaviors and Communication Attempts
Non-verbal autistic adults show pain via behaviors that untrained observers could probable push aside as unrelated autism trends or behavioral troubles instead of recognizing them as deliberate verbal exchange attempts or involuntary pain responses. Stimming escalation which includes prolonged hand flapping, rocking, spinning, or specific repetitive moves regularly indicates distress or pain instead of contentment, even though careful statement distinguishes glad stimming from distressed versions via movement quality, facial expressions, and contextual factors.
Self-injurious behaviors which include headbanging, self-biting, or self-scratching can also intensify even as humans enjoy pain they cannot otherwise communicate, representing decided attempts to override internal pain via externally generated sensation or precise frustration regarding inadequate response to their distress. Aggression toward others, assets destruction, or elopement attempts can also in addition replicate pain verbal exchange instead of primary behavioral pathology, even though safety interventions stay crucial while addressing underlying pain sources.
Some non-verbal autistic adults show modern day verbal exchange via augmentative systems which include photograph boards, virtual devices, or sign language that emergency staff sudden with the ones modalities could probably overlook. Asking caregivers about verbal exchange techniques and ensuring the ones systems stay handy for the duration of emergency department stays permits pain reporting and needs expression. Even humans without formal verbal exchange systems can also lead staff to pain sources, element to border regions, or gesture toward preferred interventions even as given opportunities and appropriate environmental modifications decreasing sensory overwhelm.
Modify Emergency Department Environment to Reduce Sensory Barriers
Environmental adjustments lowering sensory attack allow autistic sufferers to higher tolerate vital hospital treatment whilst facilitating extra correct behavioral evaluation through minimizing confounding misery from fluorescent lighting, gadget alarms, overhead announcements, and chaotic activity. Whenever possible, putting autistic sufferers in quieter remedy areas far from important nursing stations, dimming overhead lights, minimizing pointless team of workers interruptions, and lowering ambient noise extensively improves affected person cooperation and evaluation accuracy.
Allowing sufferers to put on noise-canceling headphones, sunglasses, or private garb as opposed to health facility robes respects sensory alternatives whilst keeping clinical access. Some emergency departments preserve sensory kits which include fidget tools, weighted blankets, and calming visible stimuli that offer consolation and law guide for autistic sufferers. These easy lodges exhibit appreciation for neurological variations whilst developing healing environments facilitating as opposed to impeding powerful care delivery.
A time adjustment which includes prolonged evaluation periods, appointment clustering to decrease general come upon duration, and tolerance for affected person-directed pacing whilst clinically suitable lessen cumulative sensory demands. While emergency branch performance pressures create actual constraints, pointless time compression frequently proves counterproductive through escalating behavioral responses that in the end eat extra sources through safety interventions, psychiatric consultations, and extended length-of-live as compared to start with accommodating affected person needs.
Documentation and Care Transition Considerations
Comprehensive documentation of ache evaluation methods, located behaviors, intervention responses, and powerful techniques guarantees continuity whilst care transitions among emergency nurses, consulting specialists, and inpatient units. Recording behavioral signs located as opposed to subjective ache rating assignments gives extra significant information, describing that “affected person confirmed improved rocking, facial grimacing, and tachycardia to 118 following function change, enhancing to baseline behaviors and coronary heart fee 87 thirty mins after ibuprofen administration” as opposed to arbitrarily assigning numerical ache ratings.
Discharge commands for autistic sufferers returning to network settings must consist of ache tracking steering for caregivers, figuring out behavioral adjustments warranting clinical reevaluation and imparting clean parameters for medicine administration. Written commands supplemented with visible help and caregiver teach-lower back affirmation beautifies comprehension and suitable follow-thru.
Conclusion
Pain evaluation in non-verbal autistic adults offering to emergency departments needs systematic techniques combining tested observational tools, caregiver collaboration, physiological monitoring, trauma-knowledgeable exam techniques, analgesic trials, autism-particular conduct popularity, and environmental change. Traditional self-document ache scales show insufficient for this populace whose neurological variations produce ordinary ache perception, processing, and communique requiring specialized nursing competencies.
Emergency nurses ready with evidence-primarily based totally evaluation techniques can extensively enhance ache popularity accuracy, analgesic provision equity, and standard care great for autistic sufferers who’ve traditionally skilled dismissal and insufficient symptom control. The convergence of demographic traits displaying increasing autistic grownup populations and developing emergency branch usage quotes makes autism-capable ache evaluation an important as opposed to elective nursing skill.
Healthcare establishments must prioritize team of workers education, environmental modifications, and protocol improvement making sure that each one sufferer obtains dignified, powerful ache control irrespective of communique skills or neurological characteristics. Recognizing ache as a well-known human revel in deserving compassionate reaction whilst respecting neurodevelopmental variety represents each scientific vital and moral duty for emergency nursing experts dedicated to equitable, superb care delivery.
FAQs
FAQ 1: What if caregivers aren’t gift and the affected person has no clinical statistics available?
Use tested observational tools, screen physiological parameters, behavior systematic exam noting behavioral responses, do not forget empiric analgesia trial, and call emergency contacts if identity allows. Document all evaluation tries and scientific reasoning thoroughly.
FAQ 2: How do you differentiate ache behaviors from tension or sensory overload in autistic sufferers?
Pain generally localizes to particular frame areas with exam findings, improves with analgesia, and worsens with motion or palpation. Sensory overload responds to environmental change and sensory law techniques. Both may also coexist requiring simultaneous intervention.
FAQ 3: Are there particular medicinal drugs to keep away from in autistic sufferers experiencing ache?
No absolute contraindications exist, although many autistic people reveal heightened sensitivity to aspect consequences. Start with decrease doses, screen intently for detrimental reactions, and keep away from medicinal drugs with widespread sedative or cognitive consequences whilst possible. Consult caregivers approximately preceding medicinal drug experiences.
FAQ 4: Should restraints ever be used whilst autistic sufferers face up to exam?
Physical restraint ought to be absolute ultimate hotel reserved for impending protection threats after arduous options such as environmental change, caregiver involvement, sedation, and suspending non-pressing procedures. Restraint regularly traumatizes autistic sufferers and escalates as opposed to resolving behavioral responses to ache or distress.
Read More:
https://nurseseducator.com/didactic-and-dialectic-teaching-rationale-for-team-based-learning/
https://nurseseducator.com/high-fidelity-simulation-use-in-nursing-education/
First NCLEX Exam Center In Pakistan From Lahore (Mall of Lahore) to the Global Nursing
Categories of Journals: W, X, Y and Z Category Journal In Nursing Education
AI in Healthcare Content Creation: A Double-Edged Sword and Scary
Social Links:
https://www.facebook.com/nurseseducator/
https://www.instagram.com/nurseseducator/
https://www.pinterest.com/NursesEducator/
https://www.linkedin.com/company/nurseseducator/
https://www.linkedin.com/in/afzalaldin/
https://www.researchgate.net/profile/Afza-Lal-Din
https://scholar.google.com/citations?hl=en&user=F0XY9vQAAAAJ