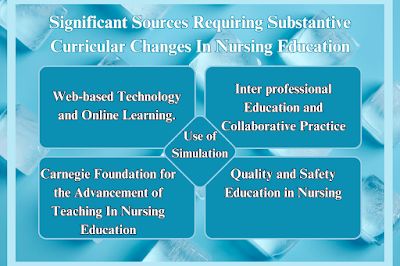
The Significant Sources Requiring Substantive Curricular Changes In Nursing Education. Several factors are demanding fundamental changes in nursing education curricula.
The Significant Sources Requiring Substantive Curricular Changes In Nursing Education
In recent years, nursing education has been profoundly influenced by a series of seminal reports, position statements, and recommendations from authoritative organizations. These sources have underscored the need for substantial curricular revisions to align with contemporary healthcare demands and to foster innovation within the field.
These include technological advances, a greater focus on health equity, changes in the healthcare landscape, and the need to adapt to changing demographics and disease patterns. Curriculum must also consider the psychological impact of health crises on healthcare professionals and promote important skills such as critical thinking and self-directed learning.
This discussion explores five critical sources driving significant curricular changes in nursing education: Quality and Safety Education for Nurses (QSEN), the Carnegie Foundation for the Advancement of Teaching, the use of simulation technology, inter-professional education and collaborative practice, and advancements in web-based technology and online learning.
Quality and Safety Education for Nurses (QSEN)
In 2001, the Institute of Medicine (IOM) released the influential report Crossing the Quality Chasm, which highlighted the urgent need for reform in health professions education to enhance quality and safety in healthcare. The report identified five core competencies essential for 21st-century health professionals: patient-centered care, teamwork and collaboration, informatics, evidence-based practice, and quality improvement, including safety (IOM, 2001).
The QSEN project was subsequently established in 2005 to ensure that nursing graduates are proficient in these competencies. The initiative aimed to integrate quality and safety competencies into nursing curricula, emphasizing faculty development to keep pace with contemporary standards. The QSEN framework, which breaks down these competencies into Knowledge, Skills, and Attitudes (KSAs), was designed to provide practical, actionable guidance for faculty.
A key element of the QSEN project was the creation of a comprehensive website to support faculty with teaching resources and strategies. This online platform aids in the dissemination of QSEN’s curricular framework and offers continuous updates and educational materials to support faculty in delivering relevant, high-quality education. The integration of QSEN content into accreditation standards ensures that nursing programs are rigorously evaluated on their incorporation of these critical competencies (Cronenwett et al., 2009).
Carnegie Foundation for the Advancement of Teaching
The Carnegie Foundation’s comparative study, The Preparation for the Professions, provided a detailed examination of professional education across various fields, including nursing. The fourth volume of this series, Educating Nurses: A Call for Radical Transformation, offers profound insights into necessary curricular changes for nursing education (Benner et al., 2010).
The study proposed four major recommendations:
- Contextual Learning: Emphasize teaching that fosters a sense of relevance and situational awareness rather than merely covering theoretical knowledge. This approach advocates for helping students “think like a nurse,” integrating real-world contexts into learning.
- Integration of Clinical and Classroom Teaching: Bridge the gap between theoretical knowledge and practical application by linking classroom instruction with clinical experiences. This recommendation aims to reflect the complex realities of modern nursing practice.
- Clinical Reasoning and Multiple Thinking Strategies: Shift the focus from generic critical thinking to encompass diverse ways of reasoning, such as clinical reasoning, clinical imagination, and scientific reasoning.
- Formation of Professional Identity: Prioritize the development of professional identity over mere role socialization. This involves creating experiential learning environments that help students internalize the essence of being a nurse.
These recommendations underscore the need for a paradigm shift in nursing education—moving from traditional content coverage to a more integrative, student-centered approach that prepares graduates for complex, real-world challenges in healthcare.
Use of Simulation
Simulation technology has dramatically transformed nursing and health professions education over the past decade. The advancement of simulation tools—ranging from low-fidelity models to high-fidelity simulators—has expanded the scope of teaching and learning strategies in nursing education.
Simulation offers students the opportunity to engage in realistic clinical scenarios in a controlled environment, enhancing their clinical skills and decision-making abilities. The expectation for simulation activities to closely resemble actual clinical settings has increased, reflecting the demand for high-quality, immersive learning experiences. These advancements have significant implications for curriculum development, necessitating the incorporation of sophisticated simulation techniques and scenarios that mirror real-world clinical environments.
Inter-professional Education and Collaborative Practice
Inter-professional education (IPE) and collaborative practice are critical components of modern healthcare delivery. Multiple reports from the Institute of Medicine (IOM) and the World Health Organization (WHO) have emphasized the importance of IPE in fostering effective teamwork and improving patient care outcomes (IOM, 2001, 2003, 2010; WHO, 2010).
In 2009, the Inter-professional Education Collaborative (IPEC) was established, comprising six national education associations from various health professions. IPEC developed core competencies for inter-professional collaborative practice, which have since been integrated into accreditation standards across health disciplines (Inter-professional Education Collaborative Expert Panel, 2011).
These competencies include:
- Teamwork and Collaboration: Developing skills for working effectively within interdisciplinary teams.
- Roles and Responsibilities: Understanding and respecting the roles of various health professionals.
- Interprofessional Communication: Enhancing communication skills to facilitate collaborative practice.
- Patient-Centered Care: Focusing on patient needs and preferences in collaborative care planning.
The integration of these competencies into nursing curricula supports the development of graduates who are prepared for collaborative, team-based patient care, addressing the evolving needs of the healthcare system.
Web-Based Technology and Online Learning
The rise of web-based technology and online learning has significantly impacted nursing education. Over the past five years, there has been a surge in the number of nursing students engaging in online or hybrid learning environments. This trend reflects the growing demand for flexible, accessible education options that accommodate diverse learning needs.
Top-tier universities and emerging institutions alike have embraced online learning, often integrating web-based technologies into traditional classroom settings to create hybrid courses. Research indicates that online learning can be as effective as traditional methods, with systematic reviews and meta-analyses showing positive outcomes in terms of student achievement, satisfaction, and cost-effectiveness (George & Shocksnider, 2014; Broome et al., 2011; Bernard et al., 2014).
The New Media Consortium’s Horizon Report highlights key trends and developments in educational technology, including the increasing use of blended learning and social media. Understanding these trends is crucial for curriculum development, ensuring that nursing programs are equipped to leverage technological advancements effectively.
Conclusion
The evolving landscape of nursing education demands a responsive and innovative approach to curriculum development. The seminal reports and recommendations discussed—ranging from QSEN to the Carnegie Foundation, simulation technology, inter-professional education, and online learning—provide critical guidance for shaping curricula that meet contemporary healthcare needs. By integrating these insights and adapting to emerging trends, nursing educators can ensure that their programs produce competent, future-ready practitioners capable of navigating the complexities of modern healthcare.
Read More:
https://nurseseducator.com/didactic-and-dialectic-teaching-rationale-for-team-based-learning/
https://nurseseducator.com/high-fidelity-simulation-use-in-nursing-education/
First NCLEX Exam Center In Pakistan From Lahore (Mall of Lahore) to the Global Nursing
Categories of Journals: W, X, Y and Z Category Journal In Nursing Education
AI in Healthcare Content Creation: A Double-Edged Sword and Scary
Social Links:
https://www.facebook.com/nurseseducator/
https://www.instagram.com/nurseseducator/
https://www.pinterest.com/NursesEducator/
https://www.linkedin.com/in/nurseseducator/
https://www.researchgate.net/profile/Afza-Lal-Din
https://scholar.google.com/citations?hl=en&user=F0XY9vQAAAAJ